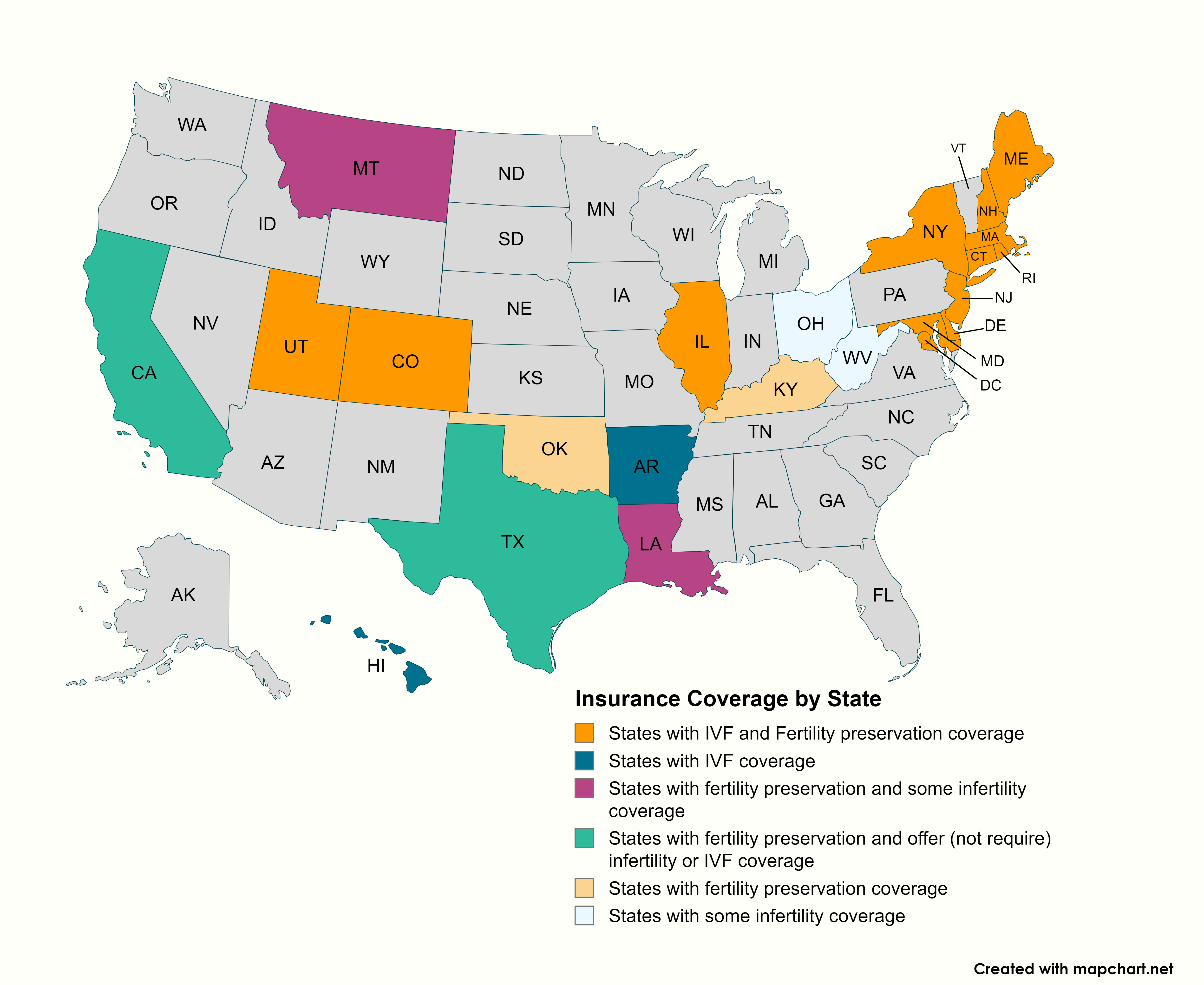
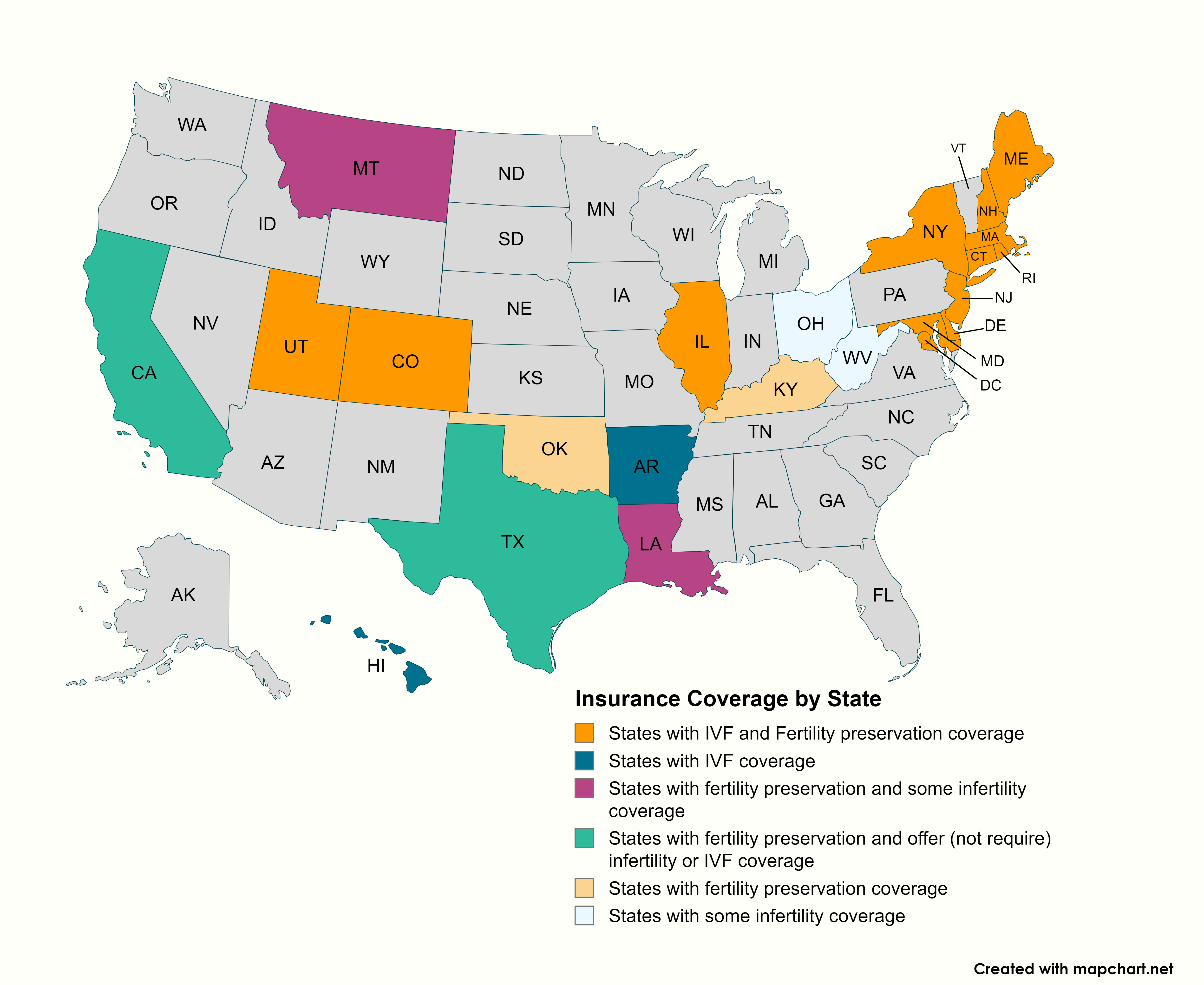
See the map below for states with an infertility insurance law. If your state is included, click on the hyperlinked state name at the bottom of the page for more details about the law and the coverage provided. We have also provided a list of questions to ask your employer to determine if you are covered by your state’s fertility insurance law or if your employer is self-insured and therefore not bound by state insurance laws. If you would like to advocate for new or expanded insurance legislation in your state, please email advocacy@resolve.org. To advocate for coverage directly with your employer, email coverageatwork@resolve.org.
Questions to ask your employer:
If you live or work in a state that has an infertility coverage law in place and want to know if you are covered by the state law, you should find out the following from your employer.
For more information on employer-provided insurance coverage, follow this link.
Summaries of State Fertility Insurance Laws
1987
Ark. Stat. Ann
Sections 23-85-137
23-86-118
Definition of Infertility/Patient Requirements
Coverage
Exceptions
1989
Cal. Health & Safety Code
Section 1374.55
Cal. Insurance Code
Section 10119.6
2019 (Fertility Preservation)
Cal. Health & Safety Code
Section 1374.551
Definition of Infertility/Patient Requirements
Coverage
Exceptions
2020 Colorado Revised Statutes, 10-16-104, (23); effective 2023.
Definition of Infertility/Patient Requirements:
Coverage
All large group (more than 100 employees) health benefit plans issued or renewed in the state on or after January 1, 2023 shall provide coverage for the diagnosis of and treatment for infertility and standard fertility preservation services, including:
The health benefits plan shall not impose:
Exceptions
(For additional information on the Connecticut law, see CT Department of Insurance Bulletin)
2005, 2017
Definition of Infertility/Patient Requirements
Coverage
Exceptions
2018 Del. Insurance Code
Title 18, Sections 1, § 3342 and Section 2, § 3556
Definition of Infertility/Patient Requirements
Coverage
All individual, group and blanket health insurance policies that provide for medical or hospital expenses shall include coverage for fertility care services, including IVF and standard fertility preservation services for individuals who must undergo medically necessary treatment that may cause iatrogenic infertility. Such benefits must be provided to the same extent as other pregnancy-related benefits and include the following:
Exceptions
1989, 2003
Hawaii Rev. Stat
Sections 431:10A-116.5
432.1-604
Definition of Infertility/Patient Requirements
Coverage
Exceptions
1991, 1997, Ill Rev. Stat. ch 215
Section ILCS 5/356m
2019, Section 215 ILCS 5/356z.29 new
2022, Section 356m. Infertility coverage. (215 ILCS 5/356m) (from Ch. 73, par. 968m)
Definition of Fertility/Patient Requirements
Coverage
Exceptions
2023 Kentucky Revised Statutes
Title 25, Chapter 304, Subtitle 17A
Definition of Infertility/Patient Requirements
Coverage
Exceptions
2001
Louisiana State Law
Subsection 215.23, Acts 2001, No. 1045, subsection
2023
Louisiana State Law, Revised Statutes 22:1036
Definition of Infertility/Patient Requirements
Coverage
Exceptions
Sec. 1. 24-A MRSA §4320-S, effective January 1, 2024
Definition of Infertility/Patient Requirements
"Infertility" means the presence of a demonstrated condition recognized by a provider as a cause of loss or impairment of fertility or a couple's inability to achieve pregnancy after 12 months of unprotected intercourse when the couple has the necessary gametes for conception, including the loss of a pregnancy occurring within that 12-month period, or after a period of less than 12 months due to a person's age or other factors. Pregnancy resulting in a loss does not cause the time period of trying to achieve a pregnancy to be restarted.
"Fertility patient" means an individual or couple with infertility, an individual or couple who is at increased risk of transmitting a serious inheritable genetic or chromosomal abnormality to a child or an individual unable to conceive as an individual or with a partner because the individual or couple does not have the necessary gametes for conception.
"Fertility preservation services" means procedures, products, medications and services, intended to preserve fertility, consistent with established medical practice and professional guidelines published by the American Society for Reproductive Medicine, its successor organization or a comparable organization for an individual who has a medical or genetic condition or who is expected to undergo treatment that may directly or indirectly cause a risk of impairment of fertility.
Coverage
A carrier offering a health plan in this State shall provide coverage to an enrollee:
Exceptions
Upon consultation with the United States Department of Health and Human Services, Centers for Medicare and Medicaid Services (CMS), the Superintendent of Insurance shall evaluate whether the coverage can be incorporated as part of the essential health benefit package or whether CMS would determine that the transfer of costs defrayed by the State to CMS would be required. The superintendent shall report by December 31, 2022 to the joint standing committee of the Legislature having jurisdiction over health coverage, insurance and financial services matters concerning its consultation with CMS and the outcome of that consultation.
MARYLAND
1985, 2000
Maryland Code Article 48A, Chapter 237
MD Insurance Code Ann. Section 15-810
MD Health General Code Ann. Section 19-701
2015-16 MD Insurance Code Ann. Section 15-810
2018 (Fertility Preservation)
Maryland Code Article 48A, Chapter 715
MD Insurance Code Ann. Section 15-801.1; Section 31-116(a)
2020
MD Insurance Code Ann. Section 15-810
Definition of Infertility/Patient Requirements
Coverage
Exceptions
1987, amended 2010
Mass Gen Laws Ann. Ch. 175, Section 47H, ch. 176A, Section 8K, ch.176B, Section 4J, ch 176G, Section 4, and 211 CMR 37.00
Definition of Infertility/Patient Requirements
Coverage
Exceptions
1987
Mont. Code Ann. Section 33-22-1521
Section 33-31-102(2)(v)
2023
Mont. Code Ann. 2-18-704
Title 33, chapter 22
Definition of Infertility/Patient Requirements
Coverage
Requires HMOs to cover infertility services as part of basic health care services.
Starting January 1, 2024, each individual and group disability policy, certificate of insurance, and membership contract that provides coverage for hospital, medical, or surgical services must cover medically necessary costs for standard fertility preservation services when an insured member is diagnosed with cancer and the standard of care involves medical treatment that may directly or indirectly cause iatrogenic infertility.
Medical assistance provided by the Montana Medicaid program also includes fertility preservation services.
Exceptions
2020 NH RSA CHAPTER 417-G
Definition of Infertility/Patient Requirements
Infertility means a disease, caused by an illness, injury, underlying disease, or condition, where an individual’s ability to become pregnant or to carry a pregnancy to live birth is impaired, or where an individual’s ability to cause pregnancy and live birth in the individual’s partner is impaired.
Standard fertility preservation services means procedures consistent with established medical practices and professional guidelines published by the American Society for Reproductive Medicine or the American Society of Clinical Oncology.
Coverage
Each health carrier that issues or renews any group policy, plan, or contract of accident or health insurance providing benefits for medical or hospital expenses, shall provide coverage for the following:
No health insurance carrier may:
Limitations on coverage shall be based on clinical guidelines and the enrollee’s medical history. Clinical guidelines shall be maintained in written form and shall be available to any enrollee upon request. Standards or guidelines developed by the American Society for Reproductive Medicine, the American College of Obstetrics and Gynecology, or the Society for Assisted Reproductive Technology may serve as a basis for these clinical guidelines.
Exceptions
Coverage does not apply to plans available through the Small Business Health Options Program (SHOP) or to Extended Transition to Affordable Care Act-Compliant Policies.
Does not cover experimental infertility procedures, non-medical costs related to third party reproduction, or reversal of voluntary sterilization. Where an enrollee is utilizing a surrogate or gestational carrier due to a medical cause of infertility unrelated to voluntary sterilization or failed reversal, the enrollee’s coverage shall not extend to medical costs relating to the preparation for reception or introduction of embryos, oocytes, or donor sperm into a surrogate or gestational carrier.
New Jersey2001, 2017, 2019, 2024
NJ Laws, Chap. 236 and supplementing Title 52 of the Revised Statutes, Section 1 of P.L.2001, c.236 (C.17:48-6x)
Definition of Infertility/Patient Requirements
COVERAGE
Group insurers, HMOs, State Health Benefits Program, and School Employees Health Benefits Program that provide pregnancy related coverage must provide infertility treatment including, but not limited to:
Exceptions
1990, 2002, 2020
NY S.B. 6257-B/A.B. 9759-B
NY Insurance Law Sections 3216 (13), 3221
FY 2020 New York State Budget
Definition of Infertility/Patient Requirements
Coverage
Group policies must provide diagnostic tests and procedures that include:
Exceptions
1991
Ohio Rev. Code Ann. Section 1751.01(A)(7)
Coverage
Exceptions
Oklahoma Statute Section 6060.8b of Title 36
Definition of Infertility/Patient Requirements
Coverage
Starting on January 1, 2025, any health benefit plan, including the Oklahoma Employees Insurance Plan, that is offered, issued, or renewed on and after the effective date of this act shall provide coverage for standard fertility preservation services only for individuals diagnosed with cancer and who are within reproductive age, when a medically necessary treatment may directly or indirectly cause iatrogenic infertility.
A health benefit plan shall not require preauthorization for coverage of standard fertility preservation services, but a health benefit plan may contain provisions for maximum benefits and may subject the covered service to the same deductible, copayment, coinsurance, and reasonable limitations and exclusions to the extent that these applications are not inconsistent with the provisions of this act.
Exceptions
1989
RI Gen. Laws sections 27-18-30, 27-19-23, 27-20-20, and 27-41-33
Revised 2006 and 2017
Definition of Infertility/Patient Requirements
Coverage
Exceptions
1987
Tex. Insurance Code Ann. Section 3.51-6, Sec. 3A
2023
Tex. Health and Safety Code. Section 1, Chapter 161
Definition of Infertilty/Patient Requirements
Coverage
Exceptions
Amends 49-20-418, as enacted by Laws of Utah 2018, Chapter 357; 63I-1-249, as last amended by Laws of Utah 2020, Chapter 98
Enacts 26-18-420.1, Utah Code Annotated 1953; 76-07-401, Utah Code Annotated 1953; 76-07-402, Utah Code Annotated 1953
Definition of Infertility/Patient Requirements
For 3-year pilot program for Public Employees’ Health Plan, 2018-2021; extended 2021-2024:
For Medicaid patients (if waiver is approved), effective January 1, 2023:
Coverage
For 3-year pilot program for Public Employees’ Health Plan, 2018-2021; extended 2021-2024:
For Medicaid patients (if waiver is approved), effective January 1, 2023:
2023 Council of the District of Columbia
70 D.C. Reg. 010351 (July 28, 2023)
Definition of Infertility/Patient Requirements
Coverage
A health insurer shall not impose:
Exceptions
1995
W.Va. Code Section 33-25A-2
Definition of Infertility/Patient Requirements
Coverage
Exception